Many state Medicaid systems today are a patchwork of vendors and capabilities not designed to pull and track data from disparate sources — a capability at the core of tracking…
Blog ()
- Home
- >
- Author: Whitney Griggs
Author: Whitney Griggs
Updated: Why ACA Premiums May Soon Become Less Affordable and What an Expiring Tax Credit Could Mean for Georgia Families

Update – August 2025: Enhanced Affordable Care Act premium tax credits (ePTCs) still expire on December 31, 2025, unless Congress acts. In 2025, Georgia Access enrolled over 1.5 million Georgians, 93% of whom depend on these subsidies to make health coverage affordable. Without an extension, premiums in Georgia are projected to jump over 75% on average, and most 2026 insurer filings already assume the credits will lapse. A typical example: a 60-year-old couple earning about $85,000 would pay roughly $18,000 more per year if the ePTCs disappear. The premium increases resulting from the expiration of the ePTCs could cause about 340,000 more Georgians to become uninsured. In short: swift Congressional action to extend the ePTCs—ideally before rate finalization—would prevent sharp premium spikes for Georgia families and avert significant coverage losses.
See how costs could rise in your Congressional district or use the calculator to estimate cost increases based on your income information — then contact your members of Congress today and tell them to extend the enhanced premium tax credits to keep health care affordable for Georgia families.
(more…)
Every year on November 1st, healthcare.gov and state-specific health insurance marketplaces open so that Americans who don’t have job-based health insurance or other coverage can shop for and enroll in health insurance. In 2024, 1.3 million Georgians enrolled in coverage in this way, and this year their marketplace will look a little different. Here’s what Georgians need to know about the changes.
Since 2013, Georgians have used healthcare.gov to view health insurance plans, qualify for financial help to lower their costs and enroll in the health plan of their choosing. In 2023, Georgia lawmakers moved to change that. The state legislature and Governor Kemp passed a new law that allows Georgia to create its state-based marketplace (SBM). Since then, the Georgia Department of Insurance has been working to create and launch Georgia Access (GeorgiaAccess.gov). Georgia Access launches November 1st.
(more…)What the Health, Georgia?
Every person who calls Georgia home deserves to live healthy and thrive. While Georgia has made recent strides to improve the health of our residents, we haven’t yet reached that goal according to Georgians themselves and our state’s health data.
To help state and community leaders make effective and informed decisions about the health and well-being of Georgians, Georgians for a Healthy Future created the illustrated What the health, Georgia guide. This publication is intended to be a reference that decision makers can go back to again and again as they consider new health laws and policies and determine how to invest public funds in health care and public health.
Download a copy of What the Health, Georgia here!
(more…)Whether you struggle with an illness like depression or addiction yourself or a person in your life does, we are all witness to the life-changing impacts of mental illness and substance use disorders. However, accessing the necessary care and treatment to manage mental illness and substance use disorders is too difficult for some Georgia families.
According to the Mental Health Association of Georgia, Georgia ranks 48th out of 50 states and D.C. for access to mental health care, resources, and insurance. Two in five Georgia children have trouble accessing the mental health treatment they need.
For years, Georgia’s mental health and substance use advocates have been working to improve access to services. While several policy wins have been achieved, the resulting changes have been modest and have not erased the biggest barriers to care.
This year is different. State legislators and advocates have named 2022 the “year of mental health.” Leaders have committed to improving access to mental health and substance use services for Georgia families.
The legislature has moved quickly on its commitment. On January 26th, House Speaker David Ralston introduced the Mental Health Parity Act. The Mental Health Parity Act is a landmark bill covering many aspects of mental health and substance use care. Topics covered in the bill range from how insurers must cover treatment to increasing the mental health and substance use provider workforce to creating mental health response teams around the state.
One of the central parts of the bill is mental health parity. Mental health parity means treating mental health and substance use services the same as physical health services, especially in how insurance companies cover these benefits. Insurers sometimes put limits on the number and types of mental health and substance use treatments that are covered but do not put those same limits on physical health treatments (like getting a broken arm fixed). This unequal treatment means that Georgians who need mental health and substance use services may have a more difficult time getting treatment and pay more for their treatment.
The Mental Health Parity Act would require insurers in Georgia to cover mental health and substance use just as they cover physical health. The bill would require private health insurers and Medicaid insurers to submit data showing that their approval and denial of mental health and substance use benefits is no more restrictive than benefits for physical care. The bill would require the state agencies that oversee private insurance and Medicaid to make it easier for consumers to file complaints if they believe their insurer is not covering mental health and substance use fairly. It will also create a full-time position dedicated to examining the data that insurers submit to make sure they are actually following the law. These measures will ensure the state has accurate data on how insurers cover these important benefits and allow the state to take action against insurers for violations.
The bill also includes steps to increase the number of behavioral health and substance use providers throughout the state, especially in rural areas. One such step is student loan forgiveness options for students training as mental health and substance use providers. Two other changes would increase Medicaid payments for certain providers, and improve data collection so state leaders will better understand the true workforce shortages.
Georgians for a Healthy Future applauds Speaker Ralston for his leadership on the Mental Health Parity Act. We support the strong provisions in the bill. The Mental Health Parity Act has been referred to the House Health and Human Services Committee, which Representative Sharon Cooper chairs. GHF will continue to provide updates as the bill moves through the legislature and look forward to working with our elected leaders to ensure all Georgia families can access the life-saving mental health and substance use treatment they need.
Want to know more? Check out this fact sheet that summarizes key pieces of the Mental health Parity Act. Share it with your family, friends, and social media networks!
Do you have a story to share about difficulties accessing mental health or substance use treatment? Share your story here. Your story can power the changes that Georgians need!
In the spring of this year, Georgians for a Healthy Future, Georgia Watch, and SOWEGA Rising launched a project in Southwest Georgia to address the burden of medical debt. Southwest Georgia, including the Albany area, experiences medical debt at a higher rate than the rest of Georgia and the country. In Dougherty County, 22% of residents have a medical debt in collections, compared to 19% for Georgia and 15% nationally. This debt also disproportionately impacts communities of color. In Dougherty County, 25% of Black residents have a medical debt in collections, compared to 21% in Georgia and 17% nationally (Urban Institute, 2020).
Medical debt can have a profound impact on the quality of a person’s life. Studies have found that medical debt is associated with a decreased use of health services, especially among low-income individuals who often become sicker while delaying care, which increases the cost of their care (Crawford, 2021). These impacts can trickle down to affect the health of the entire community.
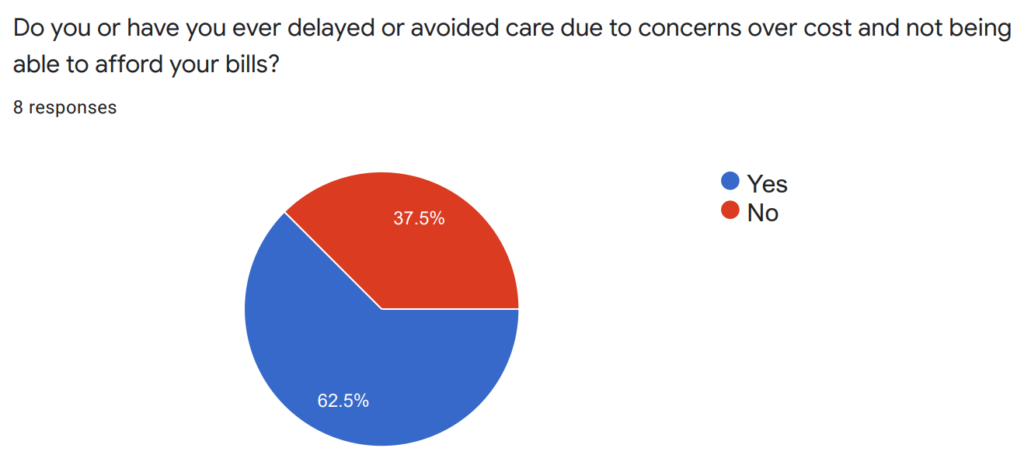
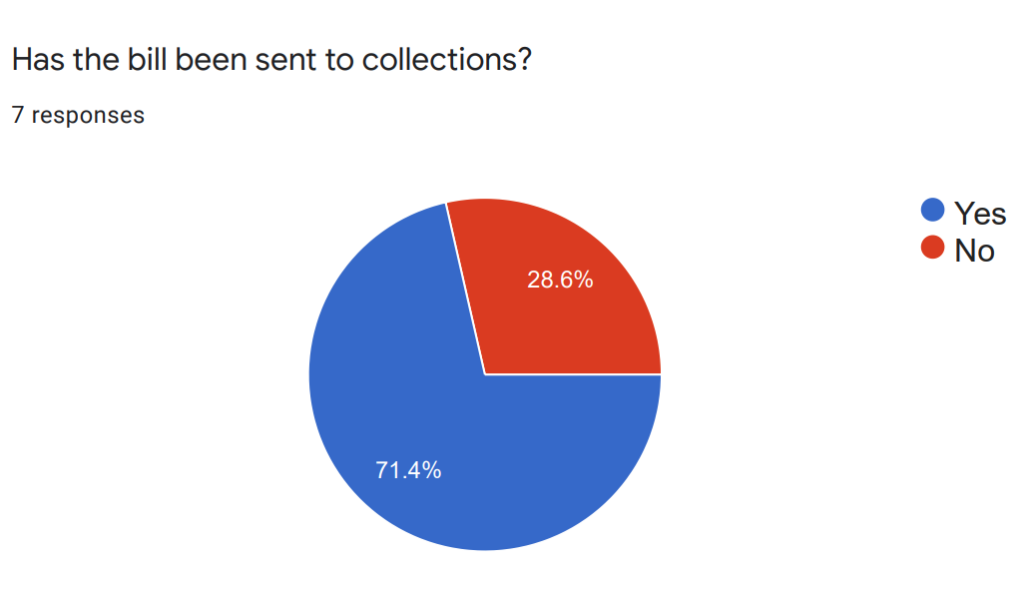
To better understand both the individual and community impacts of medical debt, Georgians for a Healthy Future, Georgia Watch, and SOWEGA Rising have used several outreach methods to invite residents of southwest Georgia to share their stories and feedback on experiences with medical debt. Since May of 2021, SOWEGA Rising has organized in-person listening sessions and Facebook Live virtual events to help individuals share their experiences with accessing and affording care in the community, including sharing whether they currently have unpaid medical bills, bills in collections, and how those bills are impacting their lives. So far, we’ve conducted seven listening sessions, and the experiences shared with us show that southwest Georgia residents are struggling to afford their care. Over 60% of those we spoke to reported delaying or avoiding care due to cost concerns, and over 70% reported an outstanding medical bill that had been sent to collections.
In October, we launched the Dish the Debt campaign in a focused effort to encourage community members, especially people of color who have been disproportionately impacted by medical debt, to share their encounters with medical bills, medical debt, and unfair debt collection practices. The campaign included social media posts throughout the month that talked about the issue of medical debt and explained why it’s so crucial for those affected by medical debt in southwest Georgia to share their story. Each post linked to a story collection form on Georgia Watch’s website where individuals could share their stories and contact information for follow-up.
A more recent effort to engage the southwest Georgia community to share their experiences with medical debt came during Georgians for a Healthy Future’s Southwest Georgia Health Care Affordability forum. During the forum, speakers from Albany Area Primary Care, Samaritan Clinic, and Valley Healthcare (local clinics that provide free or low-cost care to the community) shared how high medical costs negatively impact southwest Georgia. GHF also shared data on the disproportionate share of medical debt among communities of color in southwest Georgia during the forum. Each organization that spoke during the forum is also sharing links to the medical debt story collection form to elicit more stories from the southwest Georgia community.
Our organizations will continue to create opportunities for community feedback and stories regarding medical debt in southwest Georgia. We will ramp up our community feedback and story collection efforts in 2022, starting with a dual listening session and Affordable Care Act enrollment event in Cuthbert. We invite anyone interested to join us on January 13th, from 5 – 8 pm. Location in Cuthbert TBD.
We know that personal stories are critical to making lasting legislative and policy changes. While data on medical debt and the disproportionate impact on communities of color is deeply concerning, sharing stories creates a connection between those impacted by medical debt and Georgia’s decision-makers in a way that data cannot. We hope to use these stories, alongside data, to encourage hospital systems and lawmakers to enact policies that will protect Georgia communities from the crushing impacts of high health care costs and medical debt.
References
Crawford, K (2021). Stanford News: Stanford study finds medical debt is a double whammy for the poor. https://news.stanford.edu/2021/10/07/study-finds-medical-debt-double-whammy-poor/
Urban Institute (2020). Debt in America: An Interactive Map.https://apps.urban.org/features/debt-interactive-map/?type=overall&variable=pct_debt_collections

The high cost of medical care has long been a concern for consumers and a frequent topic of conversation among policymakers and industry leaders. Therefore, it’s no surprise to learn that many Georgians struggle to pay for health care or worry about their ability to pay for care in the future. A new survey conducted by Altarum Healthcare Value Hub, in consultation with Georgians for a Healthy Future, gives surprising new data on exactly how much Georgians struggle with the cost of healthcare.
The purpose of Altarum’s Consumer Healthcare Experience State Survey (CHESS) is to provide advocates, policymakers, and industry leaders with a better understanding of consumers’ struggles with health care costs, reveal the cost-drivers that need to be addressed in Georgia and provide support for system changes and policy solutions to improve health care affordability for consumers.
The Georgia CHESS revealed the majority of Georgians struggle with health care affordability burdens. Many Georgians are uninsured, delay needed care, or struggle to pay their medical bills due to high costs. Even more Georgians are worried about affording care in the future, especially care related to aging or medical emergencies. These results indicate the need for policymakers and stakeholders to address high costs across all areas of health care – from coverage to care to prescription drugs Additionally, consumers need more protection from high health care costs and robust, easy-to-understand tools to navigate the costs associated with care.
The survey data also unveil the need and support for Georgia lawmakers to act to relieve cost concerns for Georgians. Lawmakers can apply the CHESS results to their efforts in the 2022 legislative session, using the information to pass laws that eliminate cost as a barrier to care for Georgians, protect Georgians from rising health care costs, and require system-level changes so consumers can better tell what the true cost of their care will be.
If you would like to learn more about the Georgia results and the affordability burdens faced by Georgians, we invite you to join us on October 14th for “Coming Up Short: Affordability, Access, and Policy Fixes for Georgians,” where you’ll hear from experts about Georgia’s results and ways to address health care spending.

In June of this year, the Centers for Medicaid and Medicare Services (CMS) approved a change for Georgia’s Medicaid program that shifts how school nurses can bill for their services. Before June, Medicaid would only pay for school health services, including nursing services, if the student had a special education plan called an Individualized Education Program (IEP). IEPs are maps that lay out a program of tailored education instruction, supports, and services. These plans are required for all students receiving special education services like students with ADHD, autism, or a speech impairment. The approved change allows Medicaid to pay for more school health services provided to any student with Medicaid coverage.
(more…)CMS Requests More Information about Georgia’s Proposed Changes to Private Insurance
On June 3rd, 2021, the Centers for Medicaid and Medicare Services (CMS) sent a letter to Governor Kemp requesting additional data on the potential impacts of the Georgia Access Model. The Georgia Access Model was put forward by Kemp in his 1332 private insurance waiver, and the model would end access to healthcare.gov for Georgia consumers.
CMS is requesting additional data from the state because they believe recent changes made by President Biden’s administration to the Affordable Care Act’s health insurance marketplace have made the state’s previous analysis outdated or inaccurate. The Biden administration’s changes include:
- The COVID Special Enrollment Period (SEP)—through August 15, 2021, almost any American who does not have health insurance through their job can enroll in health coverage at healthcare.gov or by phone at 1-800-318-2596;
- More generous and expanded eligibility for Premium Tax Credits (PTCs)—almost anyone who qualifies for coverage through the ACA is now eligible for a discount on their monthly premium; and
- Increased funding for outreach and marketing for the ACA marketplace and enrollment opportunities.
These actions have led to more Americans, and Georgians, enrolling in Marketplace coverage. In addition, CMS believes that ACA enrollment would likely remain higher through 2023, when the Georgia Access Model is slated to begin.
In the letter, CMS also reasons the increase in enrollment could change insurance market dynamics enough to reduce the private sector’s incentive to enroll consumers. CMS believes with fewer uninsured people to enroll, the private sector may be less motivated to reach uninsured individuals. The idea that the private sector will be incentivized to enroll consumers once the competition of healthcare.gov is gone is a crucial assumption of Kemp’s waiver.
Georgia must now respond with updated data that takes into account the new federal changes. The new data will allow CMS to ensure the Georgia Access Model meets the protections specified in Section 1332 of the Affordable Care Act. These protections are:
- Coverage must be at least as comprehensive as Marketplace coverage;
- Coverage and protections against high costs must be as affordable as Marketplace coverage;
- A similar number of people must have coverage under the waiver as without it; and
- The waiver can’t add to the federal deficit.
The state may also request to adjust the Georgia Access Model, as needed, to meet waiver requirements in light of the new federal policies.
Once Georgia submits the new data about the Georgia Access Model, Georgia consumers, health advocates, and other stakeholders will have a chance to comment on the proposal again. CMS announced in their letter that they will hold a 30-day comment period after they receive Georgia’s new data. GHF expects the comment period will begin in early July. We will be working with our Cover Georgia partners to help Georgia individuals, organizations, and advocates comment. Stay tuned for your opportunity to weigh in again!
Stay Connected
GHF In The News
Archive
- September 2025
- August 2025
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- October 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- October 2023
- July 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- October 2022
- September 2022
- August 2022
- June 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- April 2015
- March 2015
- February 2015
- January 2015
- December 2014
- November 2014
- October 2014
- September 2014
- July 2014
- May 2014
- March 2014
- January 2014
- December 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- November 2012
- October 2012
- September 2012
- July 2012
- June 2012
- May 2012
- April 2012
- March 2012
- February 2012
- January 2012
- December 2011
- November 2011
- October 2011
- September 2011
- August 2011
- July 2011
- June 2011
- April 2011
- March 2011
- February 2011
- January 2011
- December 2010
- November 2010
- October 2010
- September 2010
- August 2010
- July 2010
- June 2010
- May 2010
- April 2010
- March 2010
- February 2010
- January 2010
- December 2009
- November 2009
- October 2009
