CMS recently announced the new special enrollment confirmation process. Under the new process, all consumers applying through the most common special enrollment periods (SEP) will need to submit documentation to verify their eligibility to use an SEP. Failure to provide supporting documents may lead to the denial of coverage. Georgians for a Healthy Future (GHF) … Read More >
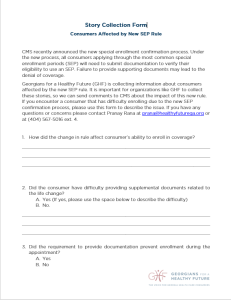
CMS recently announced the new special enrollment confirmation process. Under the new process, all consumers applying through the most common special enrollment periods (SEP) will need to submit documentation to verify their eligibility to use an SEP. Failure to provide supporting documents may lead to the denial of coverage.
Georgians for a Healthy Future (GHF) is collecting information about consumers affected by the new SEP rule. It is important for organizations like GHF to collect these stories, so we can send comments to CMS about the impact of this new rule. If you encounter a consumer that has difficulty enrolling due to the new SEP confirmation process, please use this form to describe the issue. If you have any questions or concerns please contact Pranay Rana at prana@healthyfuturega.org or at (404) 567-5016 ext. 4.